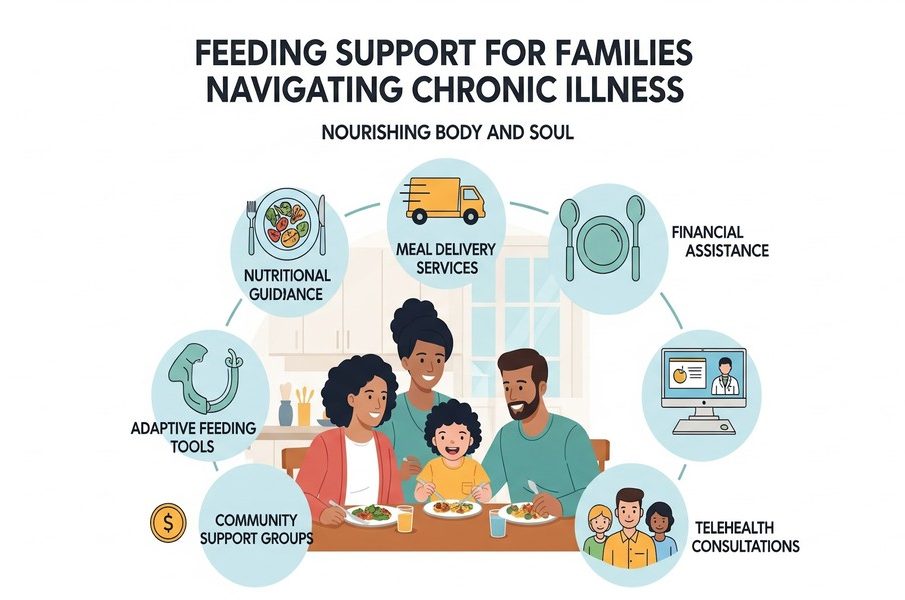
Feeding Support for Families Navigating Chronic Illness
Introduction: When Feeding and Illness Intersect
Breastfeeding and infant feeding are often imagined as natural extensions of early parenthood, but for families navigating chronic illness, feeding can become layered with uncertainty, fatigue, and emotional strain. Chronic medical conditions-whether affecting the parent, the infant, or another family member-can disrupt routines, alter physical capacity, and heighten stress during a period that already demands significant adjustment. Feeding challenges rarely exist in isolation; they are influenced by hormonal health, energy levels, medication effects, mental well-being, and access to coordinated care.
For these families, feeding success is not simply about milk supply or latch technique. It reflects a broader ecosystem of health, support, and adaptability. Understanding how chronic illness intersects with breastfeeding and infant feeding highlights the importance of collaborative care models that respect both medical complexity and family realities. When healthcare professionals work across disciplines, families are better equipped to navigate feeding decisions with confidence, flexibility, and compassion.
The Physical and Emotional Demands of Feeding During Chronic Illness
Chronic illness can place ongoing demands on the body that directly affect feeding. Conditions involving autoimmune disease, endocrine disorders, chronic pain, or metabolic dysfunction may reduce energy reserves, disrupt sleep, or interfere with milk production. Medications essential for managing long-term conditions may also influence appetite, hydration, or hormonal signaling related to lactation.
Emotionally, the pressure to feed “successfully” can intensify feelings of guilt or inadequacy for parents already coping with health challenges. Many parents report feeling torn between prioritizing their own treatment and meeting perceived expectations around feeding. This emotional tension can contribute to anxiety, depression, or burnout, further complicating feeding efforts.
Acknowledging these realities is essential. Feeding support in the context of chronic illness must be flexible, individualized, and grounded in realistic goals. Success may look different for each family, and compassionate guidance can help reframe feeding as one part of overall family health rather than a measure of parental capability.
Individualized Feeding Guidance as a Stabilizing Force
Personalized feeding support can provide stability when chronic illness introduces unpredictability. Rather than applying rigid feeding rules, individualized approaches adapt to fluctuating health, treatment schedules, and energy levels. This flexibility allows families to maintain feeding relationships without compromising medical care.
Organizations such as Corporate Lactation Services offer customized lactation support that considers complex medical backgrounds. By tailoring feeding plans to the parents’ health status, work demands, and treatment needs, lactation professionals can help families identify sustainable options-whether that involves direct breastfeeding, pumping, combination feeding, or alternative feeding methods.
Customized guidance also emphasizes problem-solving over perfection. Adjustments may be made as health changes occur, reinforcing the idea that feeding plans are dynamic. This adaptability can reduce stress, preserve bonding, and help families maintain a sense of control during prolonged medical journeys.
Hormonal Health, Energy, and Feeding Capacity
Hormonal balance plays a critical role in both feeding physiology and overall resilience. Hormones such as prolactin, oxytocin, cortisol, thyroid hormones, and sex hormones influence milk production, stress response, sleep quality, and energy metabolism. Chronic illness can disrupt these systems directly or indirectly, leading to fatigue and reduced feeding capacity.
Low energy availability is a common concern. When the body is managing inflammation, pain, or metabolic imbalance, fewer resources may be available for milk production and recovery. Addressing hormonal contributors can support feeding indirectly by improving stamina, mood stability, and physical recovery.
Understanding the hormonal dimension of feeding helps families and clinicians move beyond surface-level interventions. Rather than focusing solely on feeding mechanics, care teams can consider how systemic health influences feeding outcomes, leading to more comprehensive and sustainable support strategies.
Addressing Hormonal and Cellular Health in Complex Cases
In some families, medical support for hormonal regulation becomes an important part of maintaining functional capacity during chronic illness. Clinics such as Lions OpTimal Health focus on hormone management and cellular medicine approaches that aim to support energy levels, metabolic function, and overall vitality. While not directly related to infant feeding, these interventions may indirectly affect feeding sustainability by improving physical resilience.
When hormonal imbalances such as low testosterone, thyroid dysfunction, or adrenal stress are addressed, individuals may experience improved sleep, reduced fatigue, and enhanced capacity to engage in daily caregiving tasks. For parents navigating chronic illness, these improvements can translate into greater flexibility and endurance during feeding routines.
Importantly, such interventions are part of a broader medical strategy rather than standalone solutions. They work best when integrated with primary care oversight, feeding support, and realistic expectations around caregiving during illness.
The Role of Primary Care in Long-Term Feeding Support
Primary care providers often serve as the central coordinators for families managing chronic illness. They monitor disease progression, manage medications, and address new symptoms that may influence feeding capacity or family routines. This continuity of care is especially valuable when feeding challenges emerge over time rather than immediately postpartum.
By maintaining a comprehensive view of family health, primary care clinicians can identify when feeding difficulties are linked to broader medical changes. For example, worsening fatigue, nutritional deficiencies, or medication side effects may present first as feeding struggles. Early recognition allows for timely referrals and adjustments before stress escalates.
Primary care also plays a role in normalizing feeding adaptations. When clinicians reinforce that modified feeding plans are medically appropriate responses to chronic illness, families may feel less pressure to meet external expectations and more empowered to prioritize holistic health.
Emotional Well-Being and Feeding Relationships
Feeding is both a physical and emotional relationship. Chronic illness can alter this dynamic by introducing grief, fear, or uncertainty into daily caregiving interactions. Parents may mourn feeding experiences they had hoped for or feel disconnected from their bodies during illness.
Emotional support helps families process these feelings without assigning blame. When mental health is addressed alongside physical care, parents are better equipped to navigate feeding transitions with self-compassion. Emotional well-being also influences hormonal regulation and stress response, creating a feedback loop that affects feeding physiology.
Care teams that recognize the emotional dimensions of feeding can help families reframe success around connection, responsiveness, and adaptability rather than rigid outcomes. This perspective supports healthier long-term relationships between parents, children, and their own bodies.
Chronic Disease Management and Family Stability
Family medicine practices such as Kimball Health Services emphasize chronic disease management within the context of family systems. Ongoing conditions rarely affect only one individual; they influence routines, caregiving roles, and emotional dynamics across the household. By addressing health concerns within this broader context, primary care teams help stabilize family life.
Effective chronic disease management can reduce symptom flares, improve functional capacity, and create more predictable daily rhythms. This stability supports feeding routines, whether that involves breastfeeding schedules, pumping plans, or bottle-feeding logistics. When health is managed proactively, families may experience fewer disruptions that complicate feeding.
Additionally, family-centered care acknowledges the needs of caregivers themselves. Supporting the health of parents and partners ultimately benefits infants by creating a more resilient caregiving environment.
Collaborative Care Models That Support Feeding Goals
The most effective support for families navigating chronic illness and feeding challenges comes from collaboration. Lactation professionals, primary care providers, specialists, and wellness clinicians each contribute unique perspectives. When these professionals communicate and align their recommendations, families receive clearer guidance and more consistent support.
Collaborative care reduces the burden on families to coordinate information across providers. It also minimizes conflicting advice, which can increase stress and undermine confidence. Integrated approaches recognize that feeding success is influenced by medical stability, emotional health, and practical support.
As healthcare systems increasingly embrace multidisciplinary models, families managing chronic illness may find it easier to access coordinated feeding support that adapts to changing needs over time.
Conclusion: Feeding Support as Part of Whole-Family Care
Feeding during chronic illness is rarely a simple task, but it does not have to be an isolating one. When feeding is viewed as part of a larger health ecosystem, families gain access to support that respects both medical complexity and emotional experience. Flexible feeding plans, attention to hormonal and systemic health, and strong primary care coordination all contribute to more sustainable outcomes.
Ultimately, successful feeding is not defined by a single method or duration. It is defined by nourishment, connection, and the well-being of both parent and child. Through collaborative, compassionate care, families navigating chronic illness can find feeding solutions that align with their health realities and support long-term resilience.








